10
Impact Factor
ISSN: 1449-2288
Int J Biol Sci 2018; 14(14):2065-2072. doi:10.7150/ijbs.28608 This issue Cite
Research Paper
Comparison of Prognostic Indices in NSCLC Patients with Brain Metastases after Radiosurgery
1. Department of Radiotherapy Oncology, Chang An Hospital, Xi'an, Shaan Xi, China
2. Faculty of Health Sciences, University of Macau, Taipa, Macao SAR, China
3. Radiotherapy Department, 323 Hospital of People's Liberation Army, Xi'an, Shaan Xi, China
*These authors equally contributed to the work.
Abstract
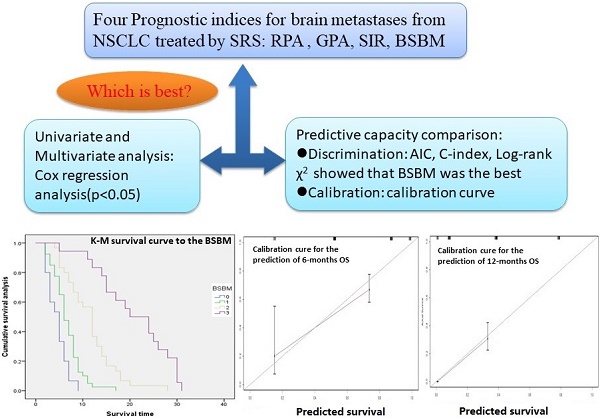
Prognostic indices are commonly used in the context of brain metastases radiotherapy to guide patient decision-making and clinical trial stratification. This study is to choose an appropriate prognostic index (PI) for non-small cell lung cancer (NSCLC) patients with brain metastases (BM) who underwent radiosurgery. A total of 103 patients with BM from NSCLC receiving radiosurgery were analyzed retrospectively. There are six prognostic factors were analyzed, including age, primary tumor control, extracranial metastasis, KPS score, number of lesions, max lesion volume; and four prognostic indices were compared, include Recursive Partitioning Analysis (RPA),Graded Prognostic Assessment (GPA), Score Index for Radiosurgery (SIR), Basic Score for Brain Metastases (BSBM). Survival curves were estimated with the Kaplan-Meier method and compared with a log-rank test stratified according to the PIs. Univariate and multivariate analysis was performed using the Cox regression analysis. The PI's predictive capacity was compared in terms of Akaike information criterion (AIC), Log-rank × 2, Concordance index (C-index) and calibration curve. The median survival time was 8 months, and the 6-months and 12-months survival rate were 61% and 26% respectively. All four prognostic indices were correlated with prognosis (P<0.005).The AIC for BSBM (686.317) was the minimum in the four PIs(range,686.317-739.113).The Log-rank × 2 value for BSBM (77.62) was the maximum in the four PIs (range,23.32-77.62).The C-index for BSBM (0.758)was superior than the other PIs predictive capacity (range,0.611-0.758). The calibration curve showed that the BSBM was able to predict 6-months and 12-months overall survival accurately. In conclusion, the BSBM may be the most accurate prognostic index for patients with BM from NSCLC who underwent radiosurgery.
Keywords: Non-small cell lung cancer, brain metastases, prognostic index, decision curve analysis, radiosurgery

 Global reach, higher impact
Global reach, higher impact