10
Impact Factor
ISSN: 1449-2288
Int J Biol Sci 2020; 16(16):3210-3220. doi:10.7150/ijbs.46896 This issue Cite
Research Paper
Postoperative adjuvant TACE-associated nomogram for predicting the prognosis of resectable Hepatocellular Carcinoma with portal vein Tumor Thrombus after Liver Resection
1. The Third Department of Hepatic Surgery, Eastern Hepatobiliary Surgery Hospital, Second Military Medical University, Navy Medical University, Shanghai 200438, China.
2. Changhai Hospital, Second Military Medical University, Navy Medical University, Shanghai 200438, China.
3. The First Department of General Surgery, Changzheng Hospital, Second Military Medical University, Navy Medical University, Shanghai 200438, China.
4. Department of Nephrology, First Affiliated Hospital, Anhui Medical University, Hefei, China.
5. Department of Gastroenterology, Anhui Provincial Hospital, University of Science and Technology of China, Hefei, 230001, China.
6. Department of Anesthesiology, Eastern Hepatobiliary Surgery Hospital, the Second Military Medical University, Shanghai, China.
*These authors have contributed equally to this work.
Abstract
Background: To explore the effects of postoperative adjuvant transarterial chemoembolization (PA-TACE) on the prognosis of HCC patients with Portal Vein Tumor Thrombus (PVTT) undergoing resection, and to develop a PA-TACE-related nomogram for predicting survival individually.
Patients and Methods: Two hundred and ninety-three consecutive HCC patients with PVTT under R0 hepatectomy were recruited. Forty-seven cases had recurrence within one month after surgery. The remaining 246 cases consisted of 90 PA-TACE and 156 non-PA-TACE cases. COX regression analysis was performed for overall survival (OS) or recurrence-free survival (RFS) of these 246 cases, allowing the derivation of independent factors that were integrated into the nomogram. C-index, calibration curves, and risk stratification were performed to evaluate the performance and discriminative power of the nomograms.
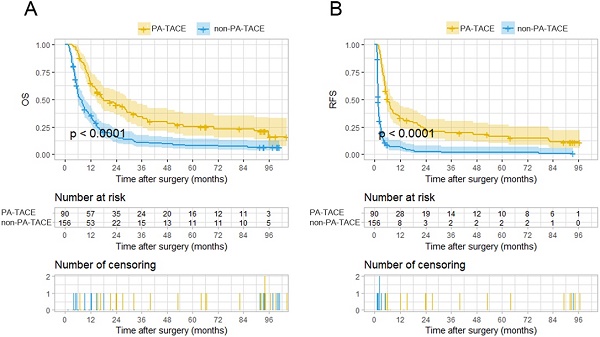
Results: In 246 patients without recurrence within one month after surgery, the OS and RFS for the PA-TACE group were significantly better than those for the non-PA-TACE group (P<0.0001, P<0.0001, respectively). After Cox regression analysis of OS or RFS, PA-TACE-related nomogram models were constructed. The C-index of the PA-TACE-related nomogram for OS and RFS was 0.72 and 0.73, respectively. Calibration curves revealed a good agreement between predictions and observations for the nomograms. Based on the nomogram-related risk stratification, Kaplan-Meier curves showed powerful discriminative ability.
Conclusions: PA-TACE therapy improved the survival of HCC patients with PVTT undergoing hepatectomy. Accurate nomogram models were developed for predicting the individual survival and recurrence of these patients.
Keywords: Postoperative Adjuvant TACE, HCC with PVTT, Hepatectomy, Nomogram, Prognosis

 Global reach, higher impact
Global reach, higher impact