10
Impact Factor
ISSN: 1449-2288
Int J Biol Sci 2022; 18(10):3934-3941. doi:10.7150/ijbs.69460 This issue Cite
Research Paper
Depressive symptoms and gender differences in older adults in Hong Kong during the COVID-19 pandemic: a network analysis approach
1. College of Education for the Future, Beijing Normal University, China.
2. Unit of Psychiatry, Department of Public Health and Medicinal Administration, & Institute of Translational Medicine, Faculty of Health Sciences, University of Macau, Macao SAR, China.
3. Institute of Advanced Studies in Humanities and Social Sciences, University of Macau, Macao SAR, China.
4. Centre for Cognitive and Brain Sciences, University of Macau, Macao SAR, China.
5. School of Nursing, Tung Wah College, Hong Kong SAR, China.
6. School of Public Health, Southeast University, Nanjing, China.
7. Center for Global Health Equity, New York University (Shanghai), Shanghai, China.
8. School of Global Public Health, New York University, NY, USA.
9. School of Nursing, The Hong Kong Polytechnic University, Hong Kong SAR, China.
10. Department of Geriatric Medicine, Beijing Tongren Hospital, Capital Medical University, Beijing, China.
11. Department of Psychiatry, The Melbourne Clinic and St Vincent's Hospital, University of Melbourne, Richmond, Victoria, Australia.
Received 2021-11-26; Accepted 2022-5-21; Published 2022-6-6
Abstract
Background: The 2019 novel coronavirus disease (COVID-19) outbreak had a detrimental impact on the mental health of older adults. This study evaluated the central symptoms and their associations in the network of depressive symptoms and compared the network structure differences between male and female older adults in Hong Kong.
Methods: Altogether, 3,946 older adults participated in this study. We evaluated the centrality indicators for network robustness using stability and accuracy tests, and examined the potential differences between the structure and connectivity of depression networks in male and female older adults.
Results: The overall prevalence of depressive symptoms was 43.7% (95% CI=40.6-46.7%) in males, and 54.8% (95% CI=53.1-56.5%) in females (P<0.05). Sad Mood, Guilt, Motor problems and Lack of Energy were influential symptoms in the network model. Gender differences were found in the network global strength, especially in the following edges: Sad Mood--Guilt, Concentration--Guilt, Anhedonia--Motor, Lack of Energy--Suicide, Appetite--Suicide and Concentration--Suicide.
Conclusions: Central symptoms in the depressive symptom network among male and female older adults may be prioritized in the treatment and prevention of depression during the pandemic.
Keywords: older adults, depression, network analysis, COVID-19, Hong Kong
Introduction
Mental health problems are common in older adults and associated with poor quality of life, impaired social functioning, and increased risk of chronic medical conditions [1]. Since the outbreak of 2019 novel coronavirus disease (COVID-19), the Hong Kong Government has adopted a variety of public health preventive measures, such as the suspension of public transport, the closure of primary and secondary schools, and a total shutdown of non-essential recreational activities (e.g., gymnasium, communal parks, sports facilities, entertainment venues) to mitigate the risks and impacts of the pandemic [2]. All these contingent measures and the ever-changing media reports on COVID-19 may increase the risk of mental health problems, worsen existing psychiatric symptoms, and heighten functional and cognitive impairments in older adults [3]. Previous studies have found that public health emergencies such as the Ebola outbreak, earthquakes, and severe acute respiratory syndrome (SARS), could trigger mental health issues [4-6]. The high prevalence of psychological morbidities has been documented among older adults who are directly or vicariously exposed to life-threatening situations [7]. Therefore, it is essential to pay special attention and provide timely interventions to this vulnerable subpopulation.
The Patient Health Questionnaire-9 (PHQ-9) is a self-report measure of depression consisting of nine items matching the Diagnostic and Statistical Manual of Mental Disorders, Fourth and Fifth Editions (DSM-IV, and -V) criteria of Major Depression [8-11]. However, depressive symptoms in older adults are heterogeneous in clinical presentation, often resulting in a highly variable manifestation of symptoms across time, especially during the COVID-19 pandemic [3, 12, 13]. Hence, it is crucial to determine the most important symptoms and the inter-relationships between depressive symptoms in older adults during the pandemic. The 'most central' symptoms can be potential treatment targets for interventions to address depression among older adults.
One of the approaches to analyzing relationships between disease symptoms is network analysis [14], an advanced framework that can also explain the onset and maintenance of psychiatric disorders [15, 16]. This approach assumes that psychiatric problems consist of co-occurring symptoms and their tendencies causally reinforce one another [17, 18]. Network analytic tools can tease out the inter-relationships between psychiatric symptoms from clinical data in a symptom network [16, 19], where each symptom is a node and may have strong associations with one another, and relate significantly to other symptoms in the network. Specific links between two symptoms are defined as edges, which represent the strength of the relationship between symptoms [20]. Node centrality index (i.e., strength, expected influence, closeness and betweenness) represents the connectedness of a given variable with all other variables in the network [21, 22]. Network analyses could examine the inter-relationships among different symptoms and their relative contributions to the model [23]. For example, in a network study conducted in European older adults, central depressive symptoms in the depressive symptom network included suicidal thoughts, depressed mood, anhedonia and pessimism [24], which might activate or perpetuate the remaining depressive symptoms. In addition, there were gender differences in the network structure. In another study on the network structure of major depressive disorder (MDD) in European older adults [25], central depressive symptoms included depressed moods, sleep difficulties, guilt and loss of interest or pleasure had fundamental roles in the network model. Further, several studies explored the network structure of depressive symptoms among other populations, such as adolescents [26, 27], college students [28], patients with other psychiatric disorders [29-31], patients with cancer and the general population [32-34].
However, findings from studies of depressive networks in other populations are not directly applicable to older adults during a pandemic, as late-life depression is often accompanied by distinctive factors, such as chronic diseases, bereavement, retirement and poor social support [12, 24, 25]. More importantly, the COVID-19 pandemic may trigger similar fear related to the 2003 SARS epidemic in Hong Kong, which killed nearly 300 people in the city [2]. In addition, epidemiological data and clinical features differed greatly between male and female older adults [35, 36], but to date, under the depression network model, the gender differences of Hong Kong older adults during the pandemic have not been examined.
Using the network analysis approach, this study evaluated the structure and gender differences of depressive symptoms (depression hereafter) among older adults in Hong Kong during the COVID-19 pandemic.
Methods
Setting and participants
This study was carried out in Hong Kong using convenience sampling in March-April 2020. The inclusion criteria were: (1) aged 50 years and above; (2) Hong Kong residents; (3) able to read and understand Chinese; (4) capable of providing electronic written consent. The data were collected with Qualtrics and Google forms based on Facebook, WeChat, and WhatsApp. The Institutional Review Board of Hong Kong Polytechnic University approved the study protocol.
Measurement
Depressive symptoms were assessed with the PHQ-9 [8]. The PHQ-9 was developed based on the 9 depressive symptom criteria in the DSM-IV. The nine items of the PHQ-9 include (1) Anhedonia (“Little interest or pleasure in doing things”), (2) Sad Mood (“Feeling down, depressed or hopeless”), (3) Sleep (“Trouble falling asleep, staying asleep, or sleeping too much”), (4) Lack of Energy (“Feeling tired or having little energy”), (5) Appetite (“Poor appetite or overeating”), (6) Guilt (“Feeling bad about yourself - or that you're a failure or have let yourself or your family down”), (7) Concentration (“Trouble concentrating on things, such as reading the newspaper or watching television”), (8) Motor (“Moving or speaking so slowly that other people could have noticed; or, the opposite - being so fidgety or restless that you have been moving around a lot more than usual”), and (9) Suicidal ideation (“Thoughts that you would be better off dead or of hurting yourself in some way”), with each item rated from 0 to 3, and a total score ranging from 0 to 27. A PHQ-9 total score of ≥5 was categorized as “having depression”, and ≥10 was considered as “having moderate to severe depression” [8].
Network estimation
The informativeness of each item was evaluated using the means of standard deviation (MSD) [28] and possible items redundancy was checked. The PHQ-9 item values of 1, 2, and 3 were converted to “presence”, while a value of 0 was labelled as “absence” of depressive symptoms.
The Ising model was used based on binary data [16, 37]. The enhanced least absolute shrinkage and selection operator (eLASSO) was adopted to regularize the models [38]. Model selection was made using the extended Bayesian Information Criterion (EBIC) [39, 40]. Each individual depressive symptom comprised nodes, and the relationships between them were edges in the model [41]. The network model was fitted with the R-package IsingFit version 0.3.1 [16].
To assess the importance of symptoms in the network, we calculated the centrality indices such as excepted influence (EI), strength, betweenness, and closeness. The accuracy and stability of the model were used to examine the robustness of the results with the correlation stability coefficient (CS-C).
Gender comparison of network characteristics
As recommended previously [24-26, 28], we investigated whether network characteristics differed between both genders. The Network Comparison Test (NCT) compared networks between male and female participants [42].
Results
Altogether, 4,464 older adults were evaluated, of whom, 3,946 participated in this study with 923 (23.4%) males and 3,023 (76.6%) females. The overall prevalence of depression (PHQ-9 total score ≥ 5) was 52.3% [95% confidence interval (CI)=50.85-53.80%)], while the prevalence of moderate-severe depression (PHQ-9 total score ≥10) was 22.2% (95% CI=21.03-23.49%). Specifically, the overall prevalence of depression was 43.7% (95% CI=40.6-46.7%) in males, and 54.8% (95% CI=53.1-56.5%) in females (P<0.05). The mean age of the participants was 56.63 [standard deviation (SD)=5.73] years and the mean PHQ-9 score was 6.03 (SD=5.47). The demographic characteristics are shown in Table 1. The PHQ-9 item scores are presented in Table S1.
Socio-demographic characteristics of the study population (N= 3,946)
| Variables | N | % |
|---|---|---|
| Gender | ||
| Men | 923 | 23.4 |
| Women | 3,023 | 76.6 |
| Married/cohabiting | 2,961 | 75.0 |
| Education level c | ||
| Elementary or below a | 55 | 1.4 |
| High school | 998 | 25.3 |
| College or higher | 2,817 | 71.4 |
| Low income b | 521 | 13.2 |
| Living alone | 162 | 4.1 |
| Mean | SD | |
| Age (years) | 56.63 | 5.73 |
| PHQ-9 total score | 6.03 | 5.47 |
Note: SD: standard deviation; PHQ-9: the 9-item Patient Health Questionnaire.
a Elementary or below = less than 7 years of education.
b Low income = low household's monthly income (< 100 hundred HKD  1.288 dollar).
1.288 dollar).
c There are missing values, therefore, the total percentage is not equal to 100%.
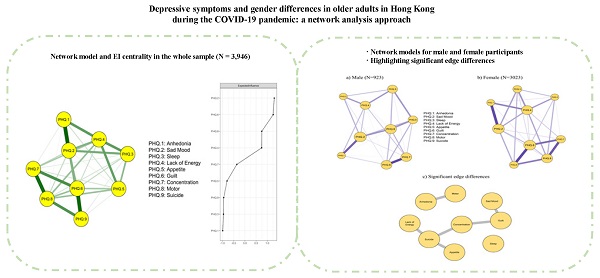
The network model of depressive symptoms was estimated (Figure 1; left panel). Strong positive correlations were found in Anhedonia-Sad Mood, Guilt-Suicide, Concentration-Motor, Guilt-Concentration, and Motor-Suicide. The numerical interactions between these symptoms were examined using a weighted adjacency matrix (Table S2). The right panel of Figure 1 shows the network's EI centrality. Symptom Sad Mood (item 2) and Guilt (item 6) showed the highest EI, followed by Motor problems (item 8) and Lack of Energy (item 4). Centrality measures including strength, betweenness and closeness are shown in Figure S1.
Strength and EI (CS-C=0.75) showed an excellent level of stability, indicating that when dropping approximately 75% of the observations, the strength index was still correlated at least 0.7 with the original network (Figure S2). The analysis of the accuracy of the edges, as implemented by means of non-parametric CIs, revealed that the precision of the edges was acceptable, with smaller CIs indicating more accurate estimations of the edges (Figure S3).
Estimated network model for dichotomized depressive symptoms and EI centrality in the whole sample (N = 3,946).
In terms of strength, Sad Mood (item 2) and Guilt (item 6) were the strongest, followed by Motor problems (item 8) and Lack of Energy (item 4) (Figure S4). Therefore, these four symptoms appeared to be particularly important and central to understanding depression among older adults in Hong Kong. Most of the comparisons were statistically significant among edge weights (Figure S5).
Descriptive statistics with frequencies of depressive symptoms by gender are shown in Table S3. Gender differences existed in the mean levels of depressive symptoms. Compared to males, females reported higher levels of Anhedonia, Sad Mood, Sleep problems, Lack of Energy, Appetite and Concentration (P <0.01).
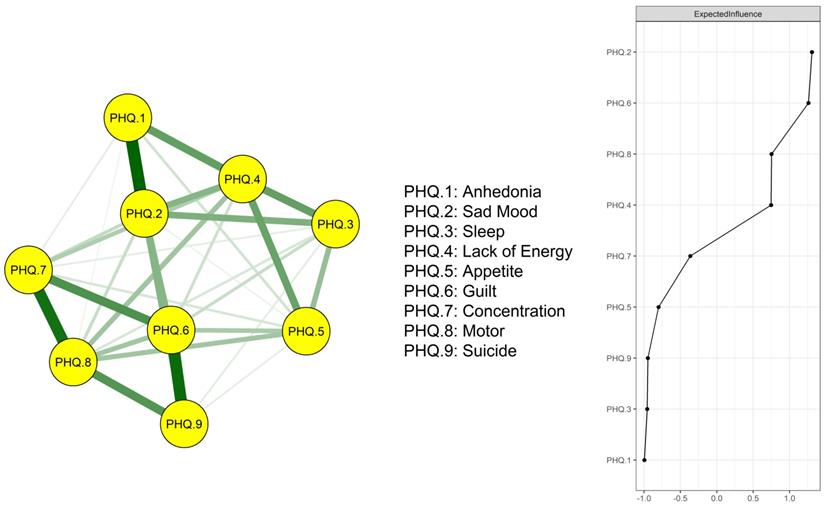
The networks for the symptoms measured by PHQ-9 for men (left panel) and women (right panel) are presented in Figure 2. Although the threshold value is equal, the network structure for men is sparser than that for women. Centrality measures for PHQ-9 items by gender groups are displayed in Figure S6. The most central symptom in women was Guilt, followed by Sad Mood and Lack of Energy. While the most central symptom in men was Sad Mood, followed by Guilt and Motor problems.
Moreover, gender differences existed in network global strength: (global strength difference=0.14, p=0.004). After testing the statistical difference of each single edge between males and females using Bonferroni-Holm correction at p < 0.05 [21], we found that the following edges between the two genders were significantly different: Sad Mood—Guilt, Concentration—Guilt, Anhedonia--Motor, Lack of Energy—Suicide, Appetite--Suicide and Concentration—Suicide (Table 2). The significant edge differences between both genders are displayed in Figure 2 (bottom panel).
Discussion
The main finding of this study was that depressive symptoms were common in older adults in Hong Kong, particularly in women. In addition, Sad Mood, Guilt, Motor problems and Lack of energy were the central nodes in the network structure that might trigger or sustain the rest of the depressive symptoms among older adults during the pandemic. Moreover, significant gender differences were found in network global strength involving the following edges: Sad Mood--Guilt, Concentration--Guilt, Anhedonia--Motor, Lack of Energy--Suicide, Appetite--Suicide and Concentration--Suicide.
In a study using network analysis on MDD among older adults in Spain, depressed mood, sleep difficulties, guilt and loss of interest or pleasure were the core symptoms [25]. In another study using network analysis among older adults in 19 European countries suicidal thoughts, sad mood, pessimism and guilt were the central symptoms of late-life depression [24]. In this study, Sad Mood, Guilt, Motor problems and Lack of Energy were the central depressive symptoms in older adults in Hong Kong, which are partly consistent with previous findings [43-45], particularly concerning Sad Mood and Guilt. Sad Mood is related to feeling down, depressed or hopeless, which is considered to be one of the core symptoms of depression [46]. In late life, sad mood may result from adverse life events (i.e., unemployment, bereavement and psychological trauma), chronic diseases, poor social support, and negative coping styles. In addition, the Hong Kong government had implemented various social distancing measures for the entire population, including mass quarantines, facility closures and restrictions on public transport [2, 47]. All these measures might inevitably decrease access to treatments for health problems in older adults, which could subsequently increase their risk of having anxiety, social isolation, and disruptions to normal routines. Guilt was another central symptom in this study, which is similar to previous findings [48]. The prevalence of chronic diseases among older people ranges from 60% to 82%, and nearly 50% of older people suffer from two or more chronic diseases [49]. Chronic diseases may increase medical and financial burden on families which, in turn, may increase guilt feelings in older adults. The financial situation may be worse if any family member was made redundant or forced to stay at home without income during the pandemic. Financial strain and exposure to unsafe and unstable environments are commonly endorsed as stressful life events among older adults [50].
Motor problems and Lack of Energy were other central symptoms in older adults, both of which were not reported in previous studies [24, 25]. The discrepancy could be due to differences in study periods (during vs. before the COVID-19 pandemic), measurements (PHQ-9 vs. other scales) and study sites (in China vs. Western countries). In this study, Motor problems refer to impairment in mobility or articulation/communication. Apart from declining physiological and cognitive functions [13, 51], older adults were often worried about the risk of infection and mortality caused by COVID-19. Older adults' concerns about higher mortality rates compared to other age groups [52] could affect their sleep quality and appetite [53], and subsequently, their energy levels. Moreover, restricted outdoor exercise due to quarantines during the pandemic could lead to a lack of energy in this subpopulation [54].
Edge differences between male and female participants
| Variable 1 | Variable 2 | P value |
|---|---|---|
| Anhedonia | Sad Mood | 0.93 |
| Anhedonia | Sleep | 0.69 |
| Sad Mood | Sleep | 0.84 |
| Anhedonia | Lack of Energy | 0.10 |
| Sad Mood | Lack of Energy | 0.46 |
| Sleep | Lack of Energy | 0.47 |
| Anhedonia | Appetite | 0.18 |
| Sad Mood | Appetite | 0.82 |
| Sleep | Appetite | 0.83 |
| Lack of Energy | Appetite | 0.61 |
| Anhedonia | Guilt | 0.93 |
| Sad Mood | Guilt | 0.02* |
| Sleep | Guilt | 0.75 |
| Lack of Energy | Guilt | 0.51 |
| Appetite | Guilt | 0.09 |
| Anhedonia | Concentration | 0.64 |
| Sad Mood | Concentration | 1.00 |
| Sleep | Concentration | 0.70 |
| Lack of Energy | Concentration | 0.69 |
| Appetite | Concentration | 0.89 |
| Guilt | Concentration | 0.03* |
| Anhedonia | Motor | 0.04* |
| Sad Mood | Motor | 0.30 |
| Sleep | Motor | 0.27 |
| of Energy | Motor | 0.50 |
| Appetite | Motor | 0.28 |
| Guilt | Motor | 0.94 |
| Concentration | Motor | 0.10 |
| Anhedonia | Suicide | 1.00 |
| Sad Mood | Suicide | 0.51 |
| Sleep | Suicide | 0.17 |
| Lack of Energy | Suicide | 0.03* |
| Appetite | Suicide | <0.001* |
| Guilt | Suicide | 0.15 |
| Concentration | Suicide | 0.01* |
| Motor | Suicide | 0.62 |
Note: Bolded values: <0.05; *significant after Bonferroni correction.
We found that the network structure of the depression model in men is sparser than in women, which is consistent with previous findings [25] and supports the notion of depressive symptoms in women as a more complex cluster of dynamic mechanisms compared to men [15]. Furthermore, the most central symptoms in women included Guilt, followed by Sad Mood and Lack of Energy, while the most central symptoms in men were Sad Mood, followed by Guilt and Motor problems, suggesting central symptoms in both genders are almost similar. However, there were significant gender differences in network global strength, as older females have a stronger connection in the following edges: Sad Mood--Guilt, Concentration--Guilt, Anhedonia--Motor, Lack of Energy--Suicide, Appetite—Suicide, and Concentration--Suicide. Older males and females might show different network structures because of psychological, physiological, and socioeconomic factors. Most epidemiological studies have reported that psychological problems are more common in women than men [35, 36]. Cognitive style often affects one's reactions to adverse events in life, and these reactions may differ based on the relationship between cognitive style and type of occurrence [55]. This may explain the differences in depressive symptoms in older females compared with older males. Women may be psychologically more affected by predicaments than men, which can result in more prevalent and severe depressive symptoms in this population. For example, previous research suggests that there is a higher prevalence of social and health related concerns among females [2]. Moreover, when facing stress and public health emergencies, women—who are often tasked with formal and informal caregiving roles and responsibilities—may be more exposed to these distressing situations compared to men [56-58].
Estimated network models for dichotomized depressive symptoms in a) male (N = 923) and b) female (N = 3,023) participants; c) highlighting significant edge differences between the male and female sample (bottom panel).
Network analysis can provide an in-depth understanding of the characteristics of depressive symptoms among older adults. Central symptoms identified in the network model may serve as targets for treatments in depression, with interventions targeting the most prominent symptoms among older adults.
The strengths of this study included a large and homogenous study sample. State-of-the-art network analyses were adopted to ensure the trustworthiness and replicability of the results. However, several limitations need to be highlighted. First, due to the study's cross-sectional design, the causal relationships between symptoms examined could not be inferred. Second, older adults with acute physical diseases and those without internet access might have been excluded in a web-based survey, which can cause selection bias. Third, no function in the NCT could control for demographic and clinical variables that differ significantly between both genders; furthermore, physical health status and anxiety symptoms were not recorded in this study, both of which may influence the findings of the gender comparisons. Finally, data were collected based on self-reports, therefore we could not exclude the possibility that some participants might have undisclosed health conditions or medical history of depression, which may bias the results.
In conclusion, our results showed that Sad Mood, Guilt, Motor problems and Lack of Energy were the most central symptoms among older adults in Hong Kong during the pandemic. Additionally, significant gender differences existed in network global strength. Our findings provide a more nuanced understanding of depression and a framework for evaluating interventions that target depression in older adults. The increased association between Lack of Energy, Suicidal thoughts and Appetite among older females appears novel and may inform new theoretical considerations for gender differences in depression. Central symptoms identified in the network model among older adults may be prioritized in the treatment and prevention of depression during the pandemic.
Abbreviations
COVID-19: The 2019 novel coronavirus disease; SARS: severe acute respiratory syndrome; PHQ-9: Patient Health Questionnaire-9; DSM-IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Editions; MDD: major depressive disorder; SD: standard deviation; eLASSO: enhanced least absolute shrinkage and selection operator; EBIC: extended Bayesian Information Criterion; EI: excepted influence; CIs: confidence intervals; CS-C: correlation stability coefficient; NCT: Network Comparison Test.
Supplementary Material
Supplementary figures and tables.
Acknowledgements
We are grateful to our research assistants and trained student helpers who assisted in the data collection process. We also thanked all the participants who participated in this study.
Author Contributions
Study design: Teris Cheung, Chee H. Ng, Yu-Tao Xiang.
Data collection, analysis and interpretation: Simon Lam, Yu Jin, He-Li Sun.
Drafting of the manuscript: Yu Jin, Teris Cheung, Chee H. Ng, Yu-Tao Xiang.
Critical revision of the manuscript: Brian J. Hall.
Approval of the final version for publication: all co-authors.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54:216-26
2. Choi EPH, Hui BPH, Wan EYF. Depression and Anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 2020 17
3. Yang Y, Li W, Zhang Q, Zhang L, Cheung T, Xiang YT. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e19
4. Taylor S. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. Newcastle upon Tyne, United Kingdom: Cambridge Scholars Publishing. 2019
5. Cénat JM, Rousseau C, Bukaka J, Dalexis RD, Guerrier M. Severe Anxiety and PTSD Symptoms Among Ebola Virus Disease Survivors and Healthcare Workers in the Context of the COVID-19 Pandemic in Eastern DR Congo. Front Psychiatry. 2022;13:767656
6. Demirchyan A, Khachadourian V, Armenian HK, Goenjian AK. The course, trajectories and predictors of depression 23 years after the 1988 Spitak earthquake in Armenia: A prospective cohort study. Psychiatry Res. 2022;313:114640
7. Vahia IV, Jeste DV, Reynolds CF 3rd. Older adults and the mental health effects of COVID-19. JAMA. 2020;324:2253-4
8. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-13
9. Martin A, Rief W, Klaiberg A, Braehler E. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. Gen Hosp Psychiatry. 2006;28:71-7
10. Bell CC. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. JAMA. 1994;272:828-9
11. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, Fifth Edition (DSM-V): American Psychiatric Publishing; 2013
12. Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961-70
13. Kok RM, Reynolds CF 3rd. Management of Depression in Older Adults: A Review. JAMA. 2017;317:2114-22
14. Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16:5-13
15. Cramer AO, van Borkulo CD, Giltay EJ, van der Maas HL, Kendler KS, Scheffer M. et al. Major Depression as a Complex Dynamic System. PLoS One. 2016;11:e0167490
16. van Borkulo CD, Borsboom D, Epskamp S, Blanken TF, Boschloo L, Schoevers RA. et al. A new method for constructing networks from binary data. Sci Rep. 2014;4:5918
17. Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91-121
18. Boschloo L, van Borkulo CD, Rhemtulla M, Keyes KM, Borsboom D, Schoevers RA. The Network Structure of Symptoms of the Diagnostic and Statistical Manual of Mental Disorders. PLoS One. 2015;10:e0137621
19. Wang Y, Hu Z, Feng Y, Wilson A, Chen R. Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Mol Psychiatry. 2020;25:3140-9
20. Epskamp S, Kruis J, Marsman M. Estimating psychopathological networks: Be careful what you wish for. PLoS One. 2017;12:e0179891
21. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav Res Methods. 2018;50:195-212
22. Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: Generalizing degree and shortest paths. Social networks. 2010;32:245-51
23. Fried EI, Nesse RM. Depression sum-scores don't add up: why analyzing specific depression symptoms is essential. BMC Med. 2015;13:72
24. Belvederi Murri M, Amore M, Respino M, Alexopoulos GS. The symptom network structure of depressive symptoms in late-life: Results from a European population study. Mol Psychiatry. 2020;25:1447-56
25. Castellanos MÁ, Ausín B, Bestea S, González-Sanguino C, Muñoz M. A Network Analysis of Major Depressive Disorder Symptoms and Age- and Gender-Related Differences in People over 65 in a Madrid Community Sample (Spain). Int J Environ Res Public Health. 2020;17:8934
26. Mullarkey MC, Marchetti I, Beevers CG. Using Network Analysis to Identify Central Symptoms of Adolescent Depression. J Clin Child Adolesc Psychol. 2019;48:656-68
27. Gijzen MWM, Rasing SPA, Creemers DHM, Smit F, Engels R, De Beurs D. Suicide ideation as a symptom of adolescent depression. a network analysis. J Affect Disord. 2021;278:68-77
28. Mullarkey MC, Stewart RA, Wells TT, Shumake J, Beevers CG. Self-Dislike and Sadness are Central Symptoms of Depression in College Students: A Network Analysis. 2018.
29. Park SC, Jang EY, Xiang YT, Kanba S, Kato TA, Chong MY. et al. Network analysis of the depressive symptom profiles in Asian patients with depressive disorders: Findings from the Research on Asian Psychotropic Prescription Patterns for Antidepressants (REAP-AD). Psychiatry Clin Neurosci. 2020;74:344-53
30. Levinson CA, Zerwas S, Calebs B, Forbush K, Kordy H, Watson H. et al. The core symptoms of bulimia nervosa, anxiety, and depression: A network analysis. J Abnorm Psychol. 2017;126:340-54
31. Beard C, Millner AJ, Forgeard MJ, Fried EI, Hsu KJ, Treadway MT. et al. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol Med. 2016;46:3359-69
32. Hartung TJ, Fried EI, Mehnert A, Hinz A, Vehling S. Frequency and network analysis of depressive symptoms in patients with cancer compared to the general population. J Affect Disord. 2019;256:295-301
33. Garabiles MR, Lao CK, Xiong Y, Hall BJ. Exploring comorbidity between anxiety and depression among migrant Filipino domestic workers: A network approach. J Affect Disord. 2019;250:85-93
34. van Rooijen G, Isvoranu AM, Kruijt OH, van Borkulo CD, Meijer CJ, Wigman JTW. et al. A state-independent network of depressive, negative and positive symptoms in male patients with schizophrenia spectrum disorders. Schizophr Res. 2018;193:232-9
35. Gu L, Xie J, Long J, Chen Q, Chen Q, Pan R. et al. Epidemiology of major depressive disorder in mainland china: a systematic review. PLoS One. 2013;8:e65356
36. Wang F, Zhang QE, Zhang L, Ng CH, Ungvari GS, Yuan Z. et al. Prevalence of major depressive disorder in older adults in China: A systematic review and meta-analysis. J Affect Disord. 2018;241:297-304
37. Barber RF, Drton M. High-dimensional Ising model selection with Bayesian information criteria. Electron J Stat. 2015;9:567-607
38. Ravikumar P, Wainwright MJ, Lafferty JD. High-dimensional Ising model selection using ℓ1-regularized logistic regression. Ann Stat. 2010;38:1287-319
39. Foygel R, Drton M. Extended Bayesian information criteria for Gaussian graphical models. Adv Neural Inf Process Syst. 2010 p. 604-12
40. Chen J, Chen Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. 2008;95:759-71
41. Epskamp S, Cramer AO, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: Network visualizations of relationships in psychometric data. J Stat Softw. 2012;48:1-18
42. van Borkulo C, Boschloo L, Borsboom D, Penninx BW, Waldorp LJ, Schoevers RA. Association of Symptom Network Structure With the Course of [corrected] Depression. JAMA Psychiatry. 2015;72:1219-26
43. Contreras A, Nieto I, Valiente C, Espinosa R, Vazquez C. The Study of Psychopathology from the Network Analysis Perspective: A Systematic Review. Psychother Psychosom. 2019;88:71-83
44. Boschloo L, van Borkulo CD, Borsboom D, Schoevers RA. A Prospective Study on How Symptoms in a Network Predict the Onset of Depression. Psychother Psychosom. 2016;85:183-4
45. van Borkulo, Boschloo L, Borsboom D, Penninx BW, Waldorp LJ, Schoevers RA. Association of Symptom Network Structure With the Course of [corrected] Depression. JAMA Psychiatry. 2015;72:1219-26
46. Mouchet-Mages S, Baylé FJ. Sadness as an integral part of depression. Dialogues Clin Neurosci. 2008;10:321-7
47. Zhao SZ, Wong JYH, Luk TT, Wai AKC, Lam TH, Wang MP. Mental health crisis under COVID-19 pandemic in Hong Kong, China. Int J Infect Dis. 2020;100:431-3
48. Kim S, Thibodeau R, Jorgensen RS. Shame, guilt, and depressive symptoms: a meta-analytic review. Psychol Bull. 2011;137:68-96
49. Wang XQ, Chen PJ. Population ageing challenges health care in China. Lancet. 2014;383:870
50. Wong SYS, Zhang D, Sit RWS, Yip BHK, Chung RY, Wong CKM. et al. Impact of COVID-19 on loneliness, mental health, and health service utilisation: a prospective cohort study of older adults with multimorbidity in primary care. Br J Gen Pract. 2020;70:e817-e24
51. Goldman DP, Cutler DM, Shang B, Joyce GF. The value of elderly disease prevention. Forum Health Econ Policy. 2006 9
52. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y. et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020;382:1199-207
53. Di Renzo L, Gualtieri P, Pivari F, Soldati L, Attinà A, Cinelli G. et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020;18:229
54. Sepúlveda-Loyola W, Rodríguez-Sánchez I, Pérez-Rodríguez P, Ganz F, Torralba R, Oliveira DV. et al. Impact of Social Isolation Due to COVID-19 on Health in Older People: Mental and Physical Effects and Recommendations. J Nutr Health Aging. 2020;24:938-47
55. Wilkinson P, Ruane C, Tempest K. Depression in older adults. BMJ. 2018;363:k4922
56. Stroud LR, Salovey P, Epel ES. Sex differences in stress responses: social rejection versus achievement stress. Biol Psychiatry. 2002;52:318-27
57. Hou F, Cerulli C, Wittink MN, Caine ED, Qiu P. Depression, social support and associated factors among women living in rural China: a cross-sectional study. BMC Womens Health. 2015;15:28 -
58. Mary-Krause M, Herranz Bustamante JJ, Héron M, Andersen AJ, El Aarbaoui T, Melchior M. Impact of COVID-19-like symptoms on occurrence of anxiety/depression during lockdown among the French general population. PLoS One. 2021;16:e0255158
Author contact
![]() Corresponding authors: Dr. Teris Cheung, School of Nursing, The Hong Kong Polytechnic University, Hong Kong; E-mail: teris.cheungedu.hk; or Dr. Yu-Tao Xiang, 3/F, Building E12, Faculty of Health Sciences, University of Macau, Avenida da Universidade, Taipa, Macau SAR, China. Fax: +853-2288-2314; Phone: +853-8822-4223; E-mail: ytxiangedu.mo; or Dr. Chee H. Ng, The Melbourne Clinic and St Vincent's Hospital, University of Melbourne, Richmond, Victoria, Australia. E-mail: cngedu.au.
Corresponding authors: Dr. Teris Cheung, School of Nursing, The Hong Kong Polytechnic University, Hong Kong; E-mail: teris.cheungedu.hk; or Dr. Yu-Tao Xiang, 3/F, Building E12, Faculty of Health Sciences, University of Macau, Avenida da Universidade, Taipa, Macau SAR, China. Fax: +853-2288-2314; Phone: +853-8822-4223; E-mail: ytxiangedu.mo; or Dr. Chee H. Ng, The Melbourne Clinic and St Vincent's Hospital, University of Melbourne, Richmond, Victoria, Australia. E-mail: cngedu.au.

 Global reach, higher impact
Global reach, higher impact